This summer, a San Francisco twitter posted a figure that shows the local COVID-19 cases were greatly underestimated.
 |
| Fig.1 |
Figure 1 shows the concentration of the SARS-CoV-2 in wastewater as dark green blocks, and publicly reported confirmed cases as red curves. Looking at the red curve would lead to the impression that the COVID-19 cases were much lower than in January, but the dark green block shows that the SARS-CoV-2 wastewater data in the San Francisco area in June and July was actually higher than in January.
At the same time, this tweet has also been echoed by twitters from all over the world, sharing Waste Water (WW) data from all over the world. Within a few hours, the Web was filled with scientific evidence of stinky shit and urine, overturning the debate on the hidden COVID-19 numbers. In fact, wastewater surveillance for the SARS-CoV-2 is not new. What is different this summer is that the public information platform is now a commonplace, providing the public with an instant understanding of the community's COVID-19 risk assessment.
 |
| Fig.2 https://biobot.io/data/ (updated 2022/10/30) |
WW profiles actually better reflect COVID-19 status than clinical PCR tests. The first known recorded case of positive RT-PCR in a poop sample was the first case in the United States at the end of January 2020 (patient day 7) [2]. The Centers for Disease Control and Prevention (CDC) launched the National Wastewater Surveillance System (NWSS) in September 2020 to coordinate wastewater surveillance programs implemented by states, tribal, local, and territorial health departments in support of the COVID-19 response. Two and a half years later, the United States has established a COVID-19 wastewater monitoring system in 46 states, 5 cities and 2 regional communities, and the samples are from wastewater systems that serve more than 130 million people in the United States [3].
As for the global context, the earliest
known result of COVID-19 wastewater surveillance is in the Netherlands in March
2020, when one or more gene fragments were detected 6 days before the first
case was reported [4].
In addition, we can know from the
CovidPoops19 project dashboard led by the University of California,
Merced, that in September 2022 the global COVID-19 wastewater monitoring
station has increased from 38 in October 2020 to 3706 now, distributed in 70
countries/ Regions, 282 academic units participation, as well as153 web-based
dashboards (Figure 3) [5]. (the moat updated numbers are in the fig 3)
 |
| Fig3. https://ucmerced.maps.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082 (updated 2022/10/30) |
SARS-CoV-2 wastewater surveillance mainly monitors shedding of SARS-CoV-2 viral fragments (genetic signals) in the feces of infected patients, whether presymptomatic, asymptomatic, or symptomatic. This waste ends up in a wastewater treatment system, where scientists can measure the number of these viral fragments in wastewater to see changes in community virus concentrations. This Environmental Surveillance (ES) method solves the so-called invisible hidden number (hidden transmission) in the face of a significant drop in COVID-19 testing or when people do not report the results of COVID-19 rapid tests at home to the health department (Figure 1. Wastewater data and clinical cases, the difference).
Sequencing wastewater to detect variants of the SARS-CoV-2 provides a better understanding of the game after the flop. For example, using RT-PCR to sequence known virus variants, or Next Generation Sequencing (NGS) sequencing of the whole genome, and then discovering unknown virus variants [6] can be used as a supplement to insufficient clinical testing, providing community answers to: Is the virus existing, absent, mutated? Concentration trends are rising or falling? etc. (Figure 2). So how did the community hidden numbers get turned out by the waste water?
First, the "public cards" ("Community Cards" in poker) are quickly turned over first. In the early stage of the pandemic, the community mostly used the strengthening of mass clinical tests to assess the coverage of the virus, but this method cost a lot of human resources and time. On the contrary, regardless of whether an individual’s trump card is covered or not (tested or not), WW data can be turned over first as a public/community card, so as to provide an overall control of the COVID-19 situation, and then in-depth prediction and prevention.
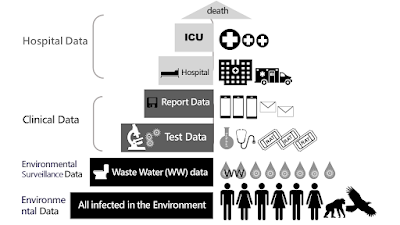
We use the seven levels of the data pyramid in Figure 4 of the WHO COVID-19 environmental surveillance document [7] to illustrate:
 |
| Fig.4 |
- the bottom layer is all viruses that are infected with the COVID-19 excreted into the environment, and
- the second layer is environmental surveillance data (ES data), including pre-symptomatic, Symptomatic or asymptomatic WW profiles.
- the third and fourth layers are clinical tests that are familiar to the public, such as RAT, PCR detection of antigens and antibodies, or diagnosis and judgment by medical personnel when testing resources are lacking;
- the last top three layers are hospitalization data, including hospitalization, severe illness and death, which are mainly monitored and reported by the medical system.
Only wastewater surveillance is currently discussed in the second layer of ES data, and it remains to be seen whether air samples in the future can be used to detect COVID-19 and other respiratory pathogens [8] as mature as wastewater surveillance. wastewater surveillance as a public health response approach is briefly as follows [6]:
1. Pathogens in feces (SARS-CoV-2 is shed in feces)
2. Sewage collection point (sewage flows to a centralized location, such as a sewage treatment plant)
3. Wastewater samples collected and transported to the laboratory (collected using a variety of methods depending on goals and resources)
4. Amplification of laboratory pathogen genetic material (concentration and amplification of genetic evidence RNA or DNA)
5. Pathogen and variant detection (PCR or NGS detection, quantification of pathogens)
6. Public Health Reporting (reporting findings to public health authorities to improve situational awareness and provide a scientific evidence base for action)
Evidence-based decisions are not only needed by government officials, but also by the general public. Early evidence of occult transmission is now recognized approximately 1 to 2 weeks earlier than clinically on average [1]. Figure 5(a) According to the WHO document, the early warning (including old and new variants) is about 2 weeks [7]:
 |
| Fig. 5 |
- Take action in Week 1 to encourage community testing,
- Predicted cases in the second week, peak hospitalization after 3 weeks of medical preparation,
- Implement interventions to reduce transmission before peak cases in week 5.
- Finally, lower the restriction measures according to the proportion of the data.
Figure 5(b) shows the COVID-19 prevention benefits of WW data at different community sizes: in community spaces with small populations such as university dormitories, naval ships, long-term care facilities, and airplanes, providing identification of early independent outbreaks; in universities, military facilities, and other population sizes In medium-sized communities, it provides notifications to allocate resources to hotspots; in metropolitan areas, it assists in large-scale outbreak surveillance.
In Taiwan, in August 2021, the surveillance stations of the SARS-CoV-2 in wastewater nationwide was expanded from 11 to 22 [8]. However, from the perspective of open science, there is no public platform for monitoring data on COVID-19 wastewater. It is like a muck that throws away the card without opening the card. Therefore, we expect that the pace of opening up Taiwan's wastewater data can keep up with the international community as soon as possible, and provide a comprehensive national COVID-19 prevention planning, community early warning, monitoring in high-risk areas such as hospitals, nursing homes, schools, or small personal travel plan evaluation information.
Is there an invisible hidden number for the COVID-19? When most people are diagnosed by RAT and have not been tested for sequencing variants, has BA.5 invaded my community? How to solve such a problem?
No more guessing, no more noisy and time-consuming and cost-intensive mass testing project, another method, COVID-19 wastewater surveillance, which is recently described by social media as shit data or poop data (poops), definitely not shit, but is instant scientific evidence that everyone submits samples to their sewer every day.
Use "wastewater sentinels" to help the community stand guard to monitor the COVID-19 and dispatch resources; see the whole picture and speculate the future trend of the epidemic in a small "crystal ball"; community sewers are like "collective intestines" that can help diagnose community conditions; Epidemic prevention without wastewater Covid-19 monitoring is "flying blindly"; and "not everyone is being tested, but everyone uses the toilet" and other recent international metaphors for Covid-19 wastewater monitoring [8], which are easy to understand and more word needed. So, is there a COVID-19 hidden number? Where are the hidden cases? The science of stinky shit and urine has the answer.
----------------------------------------------------------------------
Smelly Shit and Stinky Urine: Flip the card, a showdown with SARS-CoV-2! :
https://details-or-fragments.blogspot.com/2022/09/ww.html
----------------------------------------------------------------------
Reference:
[1] USA GAO Report, Science & Tech Spotlight: Wastewater Surveillance. GAO-22-105841 Washington, D.C.: April 11, 2022. https://www.gao.gov/products/gao-22-105841.
[2] Holshue, Michelle L., et al. "First case of 2019 novel coronavirus in the United States." New England journal of medicine (2020).
[3] US CDC, Wastewater Surveillance: A New Frontier for Public Health, https://www.cdc.gov/amd/whats-new/wastewater-surveillance.html
[4] Medema, Gertjan, et al. "Presence of SARS-Coronavirus-2 RNA in sewage and correlation withreported COVID-19 prevalence in the early stage of the epidemic in theNetherlands." Environmental Science & Technology Letters 7.7 (2020): 511-516.
[5] CovidPoops19 (Last accessed 2022/10/5) : https://ucmerced.maps.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082.
[6] Diamond, Megan B., et al. "Wastewater surveillance of pathogens can inform public healthresponses." Nature Medicine (2022): 1-4.
[7] World Health Organization. Environmental surveillance for SARS-COV-2 to complement public healthsurveillance: interim guidance, 14 April 2022. No. WHO/HEP/ECH/WSH/2022.1. World Health Organization, 2022.
[8] Related metaphors:
- SEWAGE AS SENTINEL (2022/1): https://wastewaterscan.org/wp-content/uploads/2022/01/SCAN_WastewaterScan-_Verily.pdf)
- crystal ball, flying blind (2022/8/12): https://fortune.com/2022/08/12/wastewater-surveillance-testing-sewage-future-pandemics-polio-new-york-city-covid-monkeypox-omicron/
- collective intestine (2022/9/7): https://www.economist.com/international/2022/09/07/how-covid-19-spurred-governments-to-snoop-on-sewage
- Not everyone is getting tested, but everyone is using the toilet, (2022/7/12): https://news.stlpublicradio.org/coronavirus/2022-07-12/something-in-the-water-wastewater-programs-track-covid-variants-in-missouri-flushes
[9] Taiwan CDC (Last accessed 2022/10/05) : https://www.cdc.gov.tw/Bulletin/Detail/uQz0FhPiYJbyzBXNENTRYg?typeid=9
